Uveitis / Intraocular Inflammation
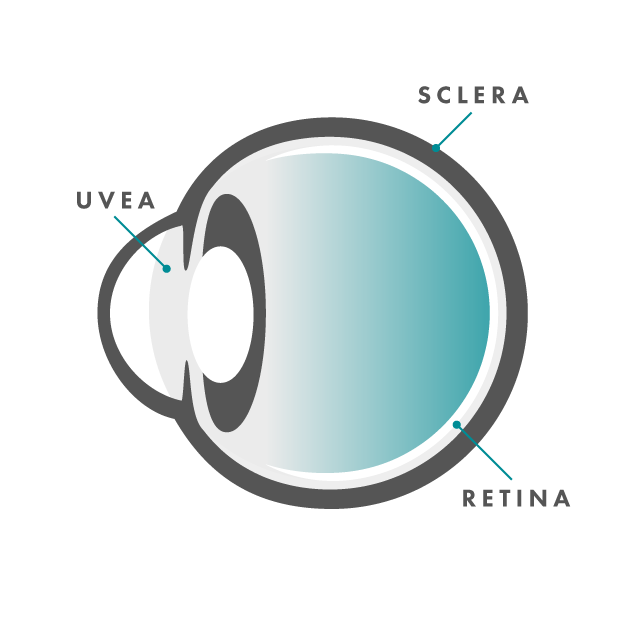
The eye can be divided into different layers:
- The outside shell of the eye is known as the sclera, and it is covered by a transparent tissue called the conjunctiva. The sclera is the white part of the eye.
- The central part of the eye is called the uvea. The uvea is made up of the iris (the colored part of the eye), the ciliary body, and the choroid layer of blood vessels.
- The inner/back layer of the eye is the retina. The retina can typically be viewed directly by your ophthalmologist though a dilated pupil.
Uveitis is an inflammation of the uvea, the middle part of the eye. However, uveitis is used as a general term to describe inflammation occurring in different parts of the eye, including in the vitreous (the clear, jelly-like substance that fills the middle of the eye between the lens and the retina), the optic nerve, and the retina.
Dr. Jiménez has extensive experience treating uveitis and works with each of his patients to help prevent additional vision problems such as severe vision loss.
Symptoms of Uveitis
Depending upon the severity and type of uveitis, you may experience varying degrees of some or all of the following symptoms:
- Eye pain / headache
- Redness of the white part of the affected eye
- Blurry vision
- Floaters or spots in the vision
- Light sensitivity
Causes of Uveitis
There are many causes of uveitis, including inflammatory/autoimmune conditions, infections, trauma, and even cancer. The location of the uveitis, whether it affects one or both eyes, and how long it has been present, can all be clues that help Dr. Jimenez to determine the underlying cause of uveitis in each particular case. In certain cases, especially in anterior uveitis, we may not be able to pinpoint the specific cause of the inflammation. This is known as “Idiopathic uveitis” or uveitis due to causes unknown.
The following are some of the conditions that may be associated with uveitis:
- Ankylosing Spondylitis
- Acute Retinal Necrosis
- Birdshot Chorioretinopathy
- Candidiasis
- Crohn’s Disease
- Cytomegalovirus
- Endophthalmitis
- Herpes Simplex/Zoster
- Inflammatory Bowel Disease
- Intermediate Uveitis/Pars Planitis
- Leukemia
- Lupus
- Lyme Disease
- Lymphoma
- Multiple Sclerosis
- Reactive arthritis
- Rheumatoid Arthritis
- Sarcoidosis
- Sickle Cell Anemia
- Syphilis
- Toxocariasis
- Toxoplasmosis
- Tuberculosis
- Vogt-Koyanagi Harada Syndrome
Diagnosing Uveitis
Dr. Jiménez will take a detailed history and perform a complete dilated eye examination as the foundation of the care he provides. Additional testing, such as OCT and Fluorescein Angiography may also be done if Dr. Jiménez determines that doing so is in his patient’s best interests. Depending on his exam findings, laboratory testing may also be ordered to help determine the cause of the uveitis.
Treating Uveitis
Any underlying conditions associated with uveitis should be evaluated and treated appropriately. Frequently a different type of physician may be consulted, such as an endocrinologist or a rheumatologist. The inflammation from the uveitis may cause a wide range of complications, including eye pain, scar tissue formation, high eye pressure inside the eye (glaucoma), and swelling in the retina (macular edema). Treatments are aimed at reducing the possibility of or eliminating these possible complications.,
Steroids, in the form of eye drops or injections in or around the eye, are commonly used to treat inflammation. In some cases, steroids may need to be surgically placed inside the eye or given orally. Dilation of the affected eye may also be used as a treatment to help alleviate pain, reduce scarring, and facilitate the healing process. In advanced cases, such as posterior uveitis, patients may also need to begin long-term treatment with immunosuppressive medications in an effort to achieve the best possible results. In cases such as these, Dr. Jiménez will work closely with your rheumatologist to determine the best treatment while minimizing any side effects from the medication.